Phimosis Treatment in Delhi
Phimosis is a condition where the foreskin is too tight to retract (pull-back) over the head of the penis. Non-surgical treatments, such as topical steroid creams or gentle stretching exercises, can often improve flexibility. For expert guidance and tailored treatment plans, visit Dr. Monga’s clinic in Delhi for comprehensive care and support.
What Is Phimosis?
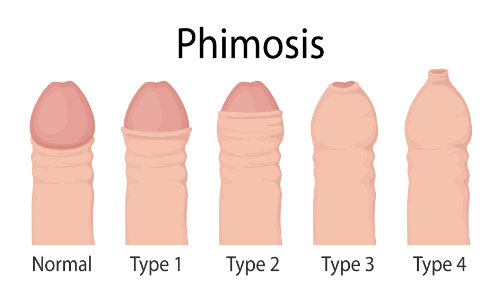
Phimosis refers to the inability to retract the foreskin from the head of the penis, a condition that only troubles uncircumcised individuals.
The foreskin, a piece of tissue covering the penis head, typically tight at birth, may be surgically removed in circumcision. Alternatively, it naturally loosens as a child matures, usually allowing full retraction for urination and cleaning by around age 6. In rare cases, tightness persists into adolescence or even develops later in life.
Phimosis vs. Paraphimosis
Phimosis may lead to a potentially hazardous condition known as paraphimosis. This occurs when the foreskin becomes trapped behind the penis head and cannot be returned to its original position. It typically arises from forcibly retracting a tight foreskin, potentially causing a cutoff of blood circulation to the penis, which requires immediate treatment.
Phimosis in adults
Phimosis is a natural occurrence in young children. In older individuals, it may result from factors such as infection, inflammation, or certain skin conditions.
Who does phimosis affect?
At birth, the foreskin (also known as the prepuce) is typically tight, but it commonly becomes looser by the age of 2. Between ages 2 and 6, it gradually loosens further and begins to detach from the penis head. Phimosis can also manifest beyond childhood.
Approximately 50 percent of boys at the age of 1 can retract the foreskin behind the glans, and this ability increases to almost 90 percent by age 3. Phimosis affects fewer than 1 percent of teenagers aged between 16 and 18.
Phimosis Causes
In older males, it affects people with:
- Recurrent urinary tract infections (UTIs)
- Infection in the foreskin
- Repeated rough handling of the foreskin
- Foreskin trauma
- It may also result from sexually transmitted infections in adults
Phimosis may manifest due to a skin condition, including:
- Eczema: It is a chronic condition characterized by itchy, red, dry, and cracked skin.
- Psoriasis: It manifests as red, flaky, and crusty patches of skin.
- Lichen planus: It is an itchy rash that can develop on various parts of the body, and it is not contagious.
- Lichen sclerosus: It results in scarring on the foreskin, potentially leading to phimosis, and it may be triggered by urinary irritation.
Phimosis Symptoms
Phimosis may not always present symptoms, but when it does, they can include redness, soreness, or swelling.
A constricted foreskin can disrupt the usual flow of urine. In severe instances, this may not allow the patient to completely empty the bladder.
Phimosis can result in penile inflammation, known as balanitis, or inflammation affecting both the glans and foreskin, termed balanoposthitis. These conditions often stem from inadequate hygiene practices.
Symptoms of balanitis include:
- Soreness, itchiness, and odor
- Redness and swelling
- Accumulation of thick fluid
- Pain while urinating
Phimosis during sexual activity can lead to discomfort, skin splitting, or reduced sensation. Using a condom and lubricant can enhance comfort during intercourse.
How is phimosis diagnosed?
When evaluating a patient, a doctor will gather a comprehensive medical history, including any past penis infections or injuries. They may also inquire about how symptoms affect sexual activity. A physical examination will involve assessing the penis and foreskin.
Additionally, the doctor may request urine tests to detect urinary tract infections or take a swab from the foreskin area to examine for bacterial presence.
Given that phimosis is associated with type 2 diabetes, adults with a constricted foreskin may undergo blood and urine tests to assess their blood sugar levels.
Phimosis Treatment
There are multiple modes of treatments available to treat phimosis. The best way to treat it is by evaluating the underlying causes and the symptoms it is presenting. Your healthcare provider may also ask you about which type of solution you would prefer to get rid of the problem.
The team of doctors at Dr Monga’s in Delhi has multiple years of experience in treating thousands of patients suffering from phimosis. If you are also experiencing similar troubles, do not delay the treatment as it may result in serious consequences.
Phimosis treatment without surgery
Treatment for phimosis in young children is typically unnecessary, as it tends to resolve naturally as the child matures and the foreskin loosens. Encouraging gentle retraction and stretching of the foreskin a few times a day, limited to a pain-free range, can facilitate this process. Bath time presents a suitable opportunity for such activities.
Here are some alternative treatment methods employed by doctors at the Dr Monga’s in Delhi depending upon your condition.
Phimosis cream
An alternative treatment option involves the use of a medicated cream or ointment applied to the foreskin multiple times daily for several weeks. Typically containing a steroid such as betamethasone, fluticasone propionate, hydrocortisone, or triamcinolone, these medications work to soften and loosen the skin and are often combined with stretching exercises.
You, however, should not start using these creams without recommendation by your doctor as they may not help you at all because of your underlying issues.
Phimosis surgery
If all treatments fail to resolve phimosis, surgical intervention may be necessary. One surgical option involves making small incisions in the foreskin to facilitate retraction. Alternatively, circumcision, which involves the complete removal of the foreskin, may be recommended.
Your doctor may suggest circumcision if you suffer from frequent infections, if there is significant scar tissue, or if the phimosis is attributed to balanitis xerotic obliterans (BXO).
What complications are related to phimosis or phimosis treatment?
Complications commonly associated with steroids, such as those related to long-term oral use, typically aren’t a concern with the creams used for foreskin retraction.
Risks associated with circumcision include:
- Bleeding
- Infection
- Improper foreskin length
- Pain
How soon will I feel better after phimosis treatment?
There is no downtime involved with the conservative ways of treatment of phimosis. Yu, however, will require seven to 10 days to completely recover after circumcision.
How can I prevent phimosis?
Physiological phimosis is typically unavoidable and is found in nearly all newborns.
However, maintaining penile hygiene is crucial. Parents or caregivers should receive guidance on the appropriate method for cleaning the penis. It is also important for them to understand that the immobility of the foreskin during the initial years of life is normal and not a cause for concern. As children become capable of self-care, they should be educated on how to clean their own penis.
Caring for an uncircumcised penis
Men with an uncircumcised penis are advised to retract the foreskin and cleanse underneath it using warm water.
Using a mild or unscented soap can help minimize the risk of irritation, as can refraining from using talc or deodorant in the area.
In most cases, uncircumcised infant boys have a foreskin that remains attached to the penis and cannot be retracted. Natural detachment typically occurs between the ages of 2 and 6, though it may take longer.
Parents should avoid attempting to force the foreskin back prematurely, as this can cause pain and damage to the foreskin.
Dos and Don’ts When Suffering from Phimosis
Dos
- It is important to regularly wash your penis using warm water or warm water combined with a mild, unscented soap.
- For adults, gently retracting the foreskin as far as possible enables thorough cleaning underneath it.
Don’ts
- Do not attempt to retract the foreskin of a baby or young boy as it may cause pain and potential damage, which could lead to issues in the future.
- Avoid using perfumed soap, talcum powder, or deodorants on your penis as they may provoke irritation.
Outlook / Prognosis
If you receive timely treatment for phimosis, particularly if it is associated with BXO, your prognosis is typically favorable.
Living With Phimosis
It is not advisable to carry on life with phimosis as the symptoms may worsen over time. Additionally, the treatment for phimosis is very simple and produces quick results.
How do I take care of myself if I have phimosis?
Whether or not you have phimosis, maintaining penile health is essential. This begins with practicing good hygiene early on by cleansing your genitals daily with mild soap and warm water. After washing, pat the penis dry gently. Ensure your hands are clean before touching your penis, and use clean underwear.
For those who are sexually active, it is advisable to use condoms and ample lubrication during intercourse. Friction during sex, particularly without a condom, may increase the risk of foreskin tearing, especially in individuals with phimosis.
When should I see my healthcare provider about phimosis?
If you have concerns about your child’s or your own foreskin mobility, it is advisable to discuss phimosis with your healthcare provider. They can provide guidance on caring for your child’s penis and address any concerns you may have. If you or your child experience difficulty urinating or encounter pain, it is important to reach out to your healthcare provider for further evaluation and assistance.
Takeaway
In conclusion, understanding phimosis is essential for maintaining penile health. From its causes and symptoms to treatment options and prevention methods, awareness is key. For specialized care, individuals can trust Dr. Monga’s in Delhi. With over 70 years of dedicated service and a team of experienced doctors, we offer personalized treatment for phimosis and related concerns.
Don’t let phimosis affect your well-being. Seek professional guidance and take proactive steps towards a healthier you at Dr. Monga’s.
FREQUENTLY ASKED QUESTIONS
Sexual intercourse is possible with phimosis, but it may not be pleasurable. Engaging in sexual activity could result in the tearing of the foreskin. To prevent this, it is crucial to use a condom and lubricant.
Physiological phimosis, occurring naturally, typically resolves on its own. Conversely, pathological phimosis, attributed to factors such as infection, scar tissue, or skin conditions, necessitates treatment.
Phimosis is often a normal aspect of a child’s development, only becoming problematic if it results in infection or urination difficulties. Additionally, it can put individuals at risk of more severe conditions.
Corticosteroid creams like 0.05% betamethasone, hydrocortisone, and triamcinolone have been employed for medical management of phimosis. Typically, these creams are applied once or twice daily for a duration of 4-8 weeks. Research indicates a success rate of 87% with this treatment approach.
A highly effective home remedy for phimosis, aiming to avoid surgery, involves gently stretching and retracting the foreskin using warm water and coconut oil. Simply pour lukewarm water over the penis, lubricate with coconut oil, and proceed to gently and gradually retract the foreskin.
Phimosis results in the prepuce trapping the penis. Consequently, following treatment, some patients perceive their penile size as significantly larger than before.
After circumcision in adults under general anesthesia with an intraoperative penile block, pain typically ranges from mild to moderate. Severe pain is uncommon and mostly associated with complications. Younger patients typically experience more discomfort.
Circumcision presents increased risks and complexities in infants older than 2 months of age and in older boys and men. Typically, circumcisions are conducted by a doctor in a hospital or outpatient office. However, they can also be performed at home by a hired professional as part of a religious or cultural ceremony.
- Choe JM. (2000). Paraphimosis: Current treatmentoptions. (http://www.drplace.com/Paraphimosis_Current_Treatment_Options.16.26276.htm)
- Monsour MA, et al. (1999). Medical management ofphimosis in children: Our experience with topical steroids. DOI: (http://dx.doi.org/10.1016/S0022-5347(01)68112-6)
- Ngan V. (2003). Balanitis. (https://www.dermnetnz.org/topics/balanitis/)
- Phimosis. (n.d.). (http://www.nationwidechildrens.org/phimosis-1)
- Phimosis. (n.d.). (https://urology.ucsf.edu/patient-care/children/phimosis)
- Phimosis and paraphimosis in children. (n.d.). (https://www.urmc.rochester.edu/encyclopedia/content.aspx?ContentTypeID=90&ContentID=P03104)
- Shahid S. (2012). Phimosis in children. DOI: (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3329654/)
- Tight foreskin. (2015). (http://www.nhs.uk/conditions/phimosis/Pages/Introduction.aspx)
- Phimosis, Adult Circumcision, and Buried Penis Treatment & Management (https://emedicine.medscape.com/article/442617-treatment?form=fpf)